Mason Woodward’s transition spanned two countries and multiple provinces. But his problems really started when he moved back home to Newfoundland and Labrador (N.L.).
The 35-year-old grew up in Happy Valley-Goose Bay, a town of 8,000 people in central Labrador. Although he knew by the age of eight he didn’t identify as a girl, it was only after going to college in Nova Scotia that he learned the term transgender, and the possibility of medical transition. After college he moved to the U.K. It was there, at the age of 30, that he began to transition. Rather than go through the U.K.’s public health care system – notorious for its years-long wait-lists – he went the private route, since he was earning a good income and could afford it. He met with a therapist and got a prescription for testosterone.
A year later his visa was up, and he returned to Canada. He relocated to Montreal, and within two months found a family doctor who specialized in trans health care. But he missed his family, so after four years in Quebec he decided to move home to Labrador. He worried, though, about what this would mean for his health care as a trans person.
The wait-list to see a doctor in Labrador was months long. Panicked, he asked both Labrador and Quebec pharmacies what he should do. Neither of them knew.
“I felt like I was giving up such a big part of me, in exchange for another big part of me,” he reflects.
His fears were confirmed when he arrived. His Quebec pharmacy had told him they could transfer his testosterone prescription to a Labrador pharmacy. But testosterone is a federally controlled substance, so when he got to Happy Valley-Goose Bay the pharmacy told him they couldn’t fulfill an ongoing Quebec prescription. The wait-list to see a doctor in Labrador was months long. Panicked, he asked both Labrador and Quebec pharmacies what he should do. Neither of them knew. And that was just the beginning of his troubles.
Gender-affirming health care inches forward
Trans people in Canada face myriad hurdles in seeking gender-affirming health care, especially when they move within the country. Because the management and delivery of health care is a provincial responsibility, each province has markedly different policies around what’s covered and how it’s provided. Underscoring these differences is the broader problem of a lack of training for medical practitioners in gender-affirming health care.
Smaller provinces face additional hurdles: most of them simply don’t have the capacity for transition-related surgeries (TRS). Even if there’s public health coverage, trans people have to navigate a confusing array of medical transport policies. These provinces are also facing the brunt of a doctor shortage.
In rural parts of the country, all these problems intersect to pose tremendous barriers to residents seeking gender-affirming health care, at a time when provinces are under pressure to improve access for a rapidly growing demographic of trans and non-binary people.
Smaller provinces face additional hurdles: most of them simply don’t have the capacity for transition-related surgeries.
Newfoundland and Labrador is a typical example. In 2019, under pressure from activists and health-care professionals, N.L. overhauled its public health policy on TRS. Previously trans people from N.L. had to go to CAMH (the Centre for Addiction and Mental Health) in Toronto to be diagnosed as having gender dysphoria – and the waiting list for this was up to seven years long. Then they would go on another waiting list for surgery. The policy overhaul finally allowed for in-province assessments and reduced the surgical wait to about two years. It also expanded coverage for additional surgeries, including two surgeries to create a penis: metoidioplasty and phalloplasty.
"But the cost of it was definitely the big deterrent for me. For a lot of people I know, the cost is what holds them back.”
But as trans Newfoundlanders began going through the system, the revised policy has come under critique. It added coverage for breast augmentation, but the criteria is the most restrictive in the country, and to date no one has qualified. Most TRS are beyond the capacity of N.L.’s health-care system, so vaginoplasty and phalloplasty patients typically go to Quebec, while chest masculinization patients typically go to New Brunswick. The province has a Medical Transportation Assistance Program (MTAP) to cover medically necessary travel, but it’s a cost-share program. Patients are expected to cover some of their travel and accommodation expenses – the exact amount is determined by a complex set of rules – and island residents must also cover a $400 deductible. If complications arise, follow-up surgery often isn’t covered at all.
Mattie Fillier has been waiting for surgery for two years. The uncertainty of waiting for a surgical date has been tough, but so is figuring out how to fund it. Both she and her fiancée work in the kitchen of a St. John’s restaurant, and she’ll need to take an extra three months off work to recover, placing added financial burdens on her fiancée. Fillier was shocked when she realized out-of-pocket surgery expenses – travel and accommodations – could run close to $5,000.
“I was like, there’s no way in hell it’s going to be able to happen. I’m not going to be able to do this. I at one point told my fiancée I’m just not going to go through with it because it’s going to cost a lot of money, it’s going to be a lot of time [off work]. She’s been my driving force behind all this – I wouldn’t be as far along in my transition if it wasn’t for her. But the cost of it was definitely the big deterrent for me. For a lot of people I know, the cost is what holds them back.”
Because the management and delivery of health care is a provincial responsibility, each province has markedly different policies around what’s covered and how it’s provided.
Fillier’s employer – an upscale gastropub in the city’s downtown – has offered to hold fundraisers, and co-workers have offered air miles to help with flights. She’s involved in the local music scene, and three fundraisers are already in the works – two punk shows and an Irish folk night.
A lot of trans people launch online fundraisers to help with medical expenses. But those only work if you have a network of friends with money to donate. Fillier launched one in March, but has only raised $30 as of the end of May.
Others rely on Hope Air – a charity that helps Canadians with medical travel and accommodations. Ironically, the charity receives support from the very provincial governments whose lack of direct funding requires residents to apply for aid. But because the charity keeps such a low profile, many don’t know about it or are hesitant to apply.
“For the longest while, I was like, I can’t do this, because of the costs,” says Fillier. “And being a low-income family, it’s definitely going to be a lot harder. Even now there’s days I second-guess whether I’m going to be able to do this. It’s not easy.”
Desperately seeking health care
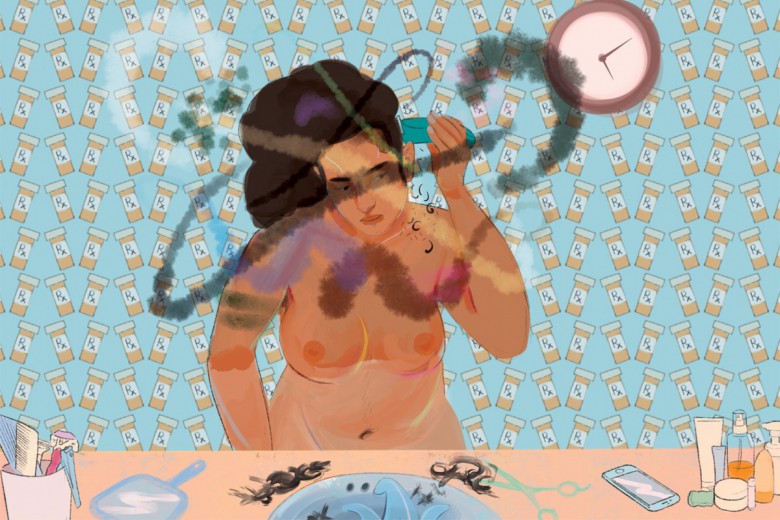
When Woodward moved back to Labrador, the problem wasn’t surgery, but what should have been a far easier matter of getting his hormone prescription filled. Eventually his former Montreal doctor agreed to send a new three-month prescription to the Labrador pharmacy but told Woodward he had to find a local solution.
Trans people taking hormones need to have regular blood work monitored by knowledgeable doctors, and this was the main concern. The few family doctors remaining in town weren’t open to taking new patients, so Woodward made an appointment at the hospital in Happy Valley-Goose Bay. It’s largely a teaching hospital, staffed in part by student residents who rotate through every couple of months. He saw two doctors there. The first gave him a testosterone prescription but said she couldn’t monitor his blood work because she didn’t know how. The second didn’t know either, and promised to learn, but she was a student and soon due to leave Labrador.
"That’s what was lacking here: being able to get past Trans 101 and really being able to talk about the nitty gritty of my ongoing health care. I want to know what I could be seeing when I’m 50, 60, 70 years old.”
Frustrated at the prospect of having to educate yet another itinerant doctor, Woodward sought other options. Planned Parenthood NL only has offices in St. John’s, but he called and asked if they could help someone in Labrador with health care needs. They agreed and set up a call with one of their doctors.
The telehealth appointment with Planned Parenthood NL exceeded his expectations. The doctor agreed to liaise with the pharmacy and blood work clinic in Labrador to monitor Woodward’s blood work remotely. He also offered the kind of trans health care advice Woodward had spent years searching for.
“He was able to tell me birth control options based on what would conflict with my hormones. We talked about menopause – as a trans man, will I be going through menopause? That’s what was lacking here: being able to get past Trans 101 and really being able to talk about the nitty gritty of my ongoing health care. I want to know what I could be seeing when I’m 50, 60, 70 years old.”
According to Planned Parenthood NL executive director Nikki Baldwin, their rotating medical staff prefer for trans patients’ health care to be handled by family physicians.
“However, N.L. is not currently in a position to provide many people with health care, let alone best-practice health care,” explains Baldwin. So the organization does what it can. Three of their seven doctors have some degree of training in hormones, and one is planning to learn.
"What’s sad is the overreliance on St. John’s. Why can’t I have a provider here [in Labrador] that I can go in and talk to, that has the same level of knowledge and the same level of resources?”
Woodward hopes the arrangement will meet his needs going forward. But he wonders what impact these hurdles have on other trans people.
“I know somebody here who’s considering transitioning, but they’re scared of navigating the system here. They don’t know how to do it,” he says. “What’s sad is the overreliance on St. John’s. Why can’t I have a provider here [in Labrador] that I can go in and talk to, that has the same level of knowledge and the same level of resources?”
Doctors “overwhelmed” with trans patients in New Brunswick
The primary health-care crisis is acute in Atlantic Canada, particularly so in nearby New Brunswick.
While the region struggles to retain physicians, Dr. Adrian Edgar is one doctor who came back. Having spent summers growing up in New Brunswick, he practised in B.C. before returning in 2015 to open a family practice in Fredericton. The numbers of trans patients who showed up far exceeded his expectations.
“It was overwhelming, to be honest,” he says. “If you look at the numbers of what we would predict for trans people in the world, you wouldn’t expect New Brunswick to have had the volume of people we were treating. I really didn’t think I would have such a large practice. Hundreds of trans people came through the clinic.”
“If we aren’t valuing queer and trans health in medical education, in medical schools, then people are going to feel that it’s either not important or that they’re under-skilled or under-trained or incompetent and therefore they’re not going to go into the field.”
His practice – Clinic 554 – quickly became a cherished institution in the small province. But because N.B. refuses to fund abortions outside of hospitals, they took up the lion’s share of his overhead costs and he was forced to close in 2020.
Edgar says it’s important to develop a funding model that recognizes the realities of trans health care. “Doctors are more likely to get involved in things that pay the bills,” he says. When a trans person first sees a doctor, it’s not like someone asking about a bump on their foot.
“It’s a person who for the first time is talking about gender and if they have dysphoria, or comorbid struggles related to gender – maybe they have been involved in sex work but not voluntarily, maybe they were kicked out of their house, maybe they did struggle with addiction – if you’ve got all these ancillary things that people are talking about, it’s not a one-minute visit,” Edgar explains.
"That’s medically essential health care. But that doesn’t matter to men who don’t care about the safety or mental well-being of a feminine person.”
Physicians in Canada operate much like small businesses, invoicing governments for the services they provide based on provincial fee codes. When Edgar worked as a street doctor in Vancouver, the B.C. government had a complex care fee code that recognized the complexity of his having to find patients without homes and work with them to identify their pressing medical needs – one patient might take up an entire afternoon. New Brunswick doesn’t have that, but it does have age-stratified add-on fee codes providing extra compensation for elderly patients. And doctors get an annual bonus for every patient in their clinic with diabetes.
“So there is a model […] that would incentivize family doctors to do trans complex care, but we don’t have it for trans people in New Brunswick,” he says. “I think they would have to have either an add-on fee code, or some kind of complex care fee code that would allow you to spend time with the patient to make them feel like they can open up to you and be authentic.”
There are plenty of ideas out there for improving trans health care, but not a lot of action. Why not?
“I think that misogyny underlies a lot of the problems in health care,” says Edgar. “There’s generalized misogyny across everything. Across the country we will pay publicly for vaginoplasty, but we won’t pay for facial feminization surgery. Or tracheal shave, or breast implants. I think that’s very misogynistic because it’s underpinned by the idea that in order to be a woman you should have something that a man can put his penis in. That’s basically what underlies that. As opposed to listening to trans-feminine people about what makes them feel safe and seen. And if that would be maybe a change in their brow ridge or their Adam’s apple or their jaw line, then obviously that is essential. That’s medically essential health care. But that doesn’t matter to men who don’t care about the safety or mental well-being of a feminine person.”
"I really didn’t think I would have such a large practice. Hundreds of trans people came through the clinic.”
Dr. Mari-Lynne Sinnott practises as a primary care physician in St. John’s. When she opened her first clinic in 2015 she had about a dozen trans patients. Seven years later, she has over 600. She’s been working with the local medical school to expose more students to trans health care. But part of the problem, she says, is lack of financial incentives for physicians to get involved in trans health care. Edgar agrees.
“If we aren’t valuing queer and trans health in medical education, in medical schools, then people are going to feel that it’s either not important or that they’re under-skilled or under-trained or incompetent and therefore they’re not going to go into the field,” he says.
“It’s a misconception that doctors don’t want to do trans health,” Edgar continues. “I think generally doctors do want to serve trans people, but they don’t feel that they can do it as well as they expect themselves to be able to and then they’re embarrassed or they’re ashamed, and then they carry that into the encounter and then they just want to get it over with as quick as possible and hand the person off to someone else, because they don’t want to admit that they’re not good at something. It’s just that professional kind of culture.”
Yukon’s “gold standard”
In 2021, Yukon introduced a new policy on gender-affirming health care that has been celebrated as the best in North America. It covers not just top and bottom surgery, but facial feminization surgery, tracheal shave, laser hair removal, and electrolysis, among other things.
Mira Sirois, communications manager with Queer Yukon, says that while the policy is “on paper the best trans health care coverage you can get in North America,” Yukon’s government developed the policy “without much thought or analysis on the how.” That’s led to a scramble to figure out how to implement it. Yukon brought in a World Professional Association for Transgender Health team to train local health practitioners. But because there are not enough service providers within Yukon, patients still have to travel outside the territory to access services – such as hair removal, which requires regular sessions – and that creates logistical and funding problems.
“We need more access to resources within the territory,” says Sirois. “We really need more doctors.”
“Either provide the resources in every province and territory or somehow create a system that manages it more effectively at the federal level.”
Yukon does have significant advantages over other rural jurisdictions: a fully covered medical travel program, which allows access to clinics in multiple provinces for top and bottom surgeries.
But the logistics of connecting patients to services remains a problem, says Sirois, who feels the country needs a federal policy or agency to coordinate trans health care.
“Either provide the resources in every province and territory or somehow create a system that manages it more effectively at the federal level.”
In principle, Edgar and Sinnott like the idea of greater federal coordination. But they also underscore that patient autonomy and choice are supposed to be part of Canadian health care – allowing patients to review different clinics and techniques and decide those they feel most comfortable with.
“Policies are often created with the expectation that people who want the service will fit themselves into the policy,” says Sinnott. “There is no one-size-fits-all approach to transition. It’s an intensely personal experience and people should be supported in their individual journey. This includes having the autonomy to access surgery when they need it, how they need it, from the provider that they choose. My concern is that the more regulation there is, the less autonomy trans folks may have in how they access service and from whom.”
“We need more access to resources within the territory,” says Sirois. “We really need more doctors.”
However it’s difficult to balance principles with practice in an under-resourced system.
Some practitioners look with envy to provinces like British Columbia or Ontario, which have provincially coordinated trans health care. Trans Care BC and Rainbow Health Ontario are both provincially funded health-care organizations that coordinate trans health care in those provinces, helping patients navigate the system by matching them up with the services and providers they need. In smaller provinces, individual clinicians are struggling to do that job themselves.
Patient demand is surging in an already strained system
In April, Statistics Canada released the first official data on trans and non-binary demographics in Canada, drawn from new census questions introduced in 2021. The data confirmed what doctors like Edgar and Sinnott have been saying: demand for gender-affirming health care is huge in smaller provinces and territories. Yukon reported the second highest proportionate gender diversity in the country. NL is tied for the third-highest proportion of transgender women and third-highest proportion of transgender men. And, per capita, Fredericton is the third most gender diverse urban centre in Canada – ahead of Toronto, Montreal, and Vancouver.
Yet it’s smaller jurisdictions like these where trans health care is most precarious. Nova Scotia led the country in its proportion of trans and non-binary people, and per capita Halifax is the second-most gender diverse Canadian urban centre. Yet in May the province’s only TRS surgeon announced he would no longer provide those surgeries, blaming the province for its refusal to designate “appropriate” fee codes for TRS. In addition, two endocrinologists who provide referrals that are mandatory to access TRS announced they would no longer accept new clients, saying they don’t have the capacity.
"Maybe it’s in St. John’s or maybe it’s in Halifax, but there should be an Atlantic centre.”
Jack Woodman is vice-president of strategy, quality, risk, and privacy at Women’s College Hospital (WCH) in Toronto. They helped oversee the development of that hospital’s new TRS unit, which, due to capacity issues, has only accepted Ontario patients to date. When Ontario simplified the process to access TRS in 2016, WCH anticipated the surgical bottleneck that would result, and it began developing its own TRS unit. Woodman suggests it’s time for the Atlantic provinces to take a serious collective look at how TRS is offered in that region.
“For [Atlantic Canadian patients], should they have to travel to Montreal or Ontario? No. […] There should be an Atlantic centre that provides access on the East Coast. Maybe it’s in St. John’s or maybe it’s in Halifax, but there should be an Atlantic centre.”
Organizing from the ground up
In response to a lack of institutional supports in all three jurisdictions, a vibrant array of grassroots community groups has blossomed to meet the need. Queer Yukon is renovating a physical space into which it hopes to move in the coming months. In Newfoundland and Labrador, Quadrangle is campaigning to create a provincial 2SLGBTQIA+ community centre, while Trans Support NL operates peer support groups across the island as well as Labrador. In Nova Scotia, a new mobilization is underway to expand care in that province, spearheaded by groups like Gender Affirming Care Nova Scotia.
And New Brunswick’s queer and trans activists are on fire. The roster is impressive for a small province: in addition to local Pride organizations, there’s also Imprint Youth Association, Fredericton Gender Minorities, UBU Atlantic, QT Fatties in NB, Transgender Care Moncton, and more.
“There is a lot of co-support happening,” says Imprint member Nikki Lyons-MacFarlane. “It’s a really great community here. Despite lack of access, it’s really great and booming.”
“I want to see transition-related care just become an understood aspect of primary care."
“It really is a booming time for LGBT groups in New Brunswick,” says Imprint co-founder Reid Lodge. The solution to a lack of institutional support is to build community resilience and strong mutual support networks, they say.
“It’s way more important to connect with the community right now and do whatever we can do to support the community. Wasting our time emailing the premier is not going to get us anywhere.”
But the group has received support from the federal government. Earlier this year, Imprint received a grant from Women and Gender Equality Canada for a gender-affirming health-care project. The 25-month project will develop a training program for primary care providers. It’s the sort of incentive for training that Sinnott feels is needed.
“I want to see transition-related care just become an understood aspect of primary care,” she says. “Just like we do contraception with cis females or hormone replacement therapy for post-menopausal women. I would like to see more family doctors feeling empowered to do this in their regular practice. It should be a service that you can provide to your patients just like you would treat a toenail infection or anything else.”
This article was the recipient of the 2022 Andrea Walker Memorial Fund for Feminist Health Journalism.




_780_520_90_s_c1.jpg)
