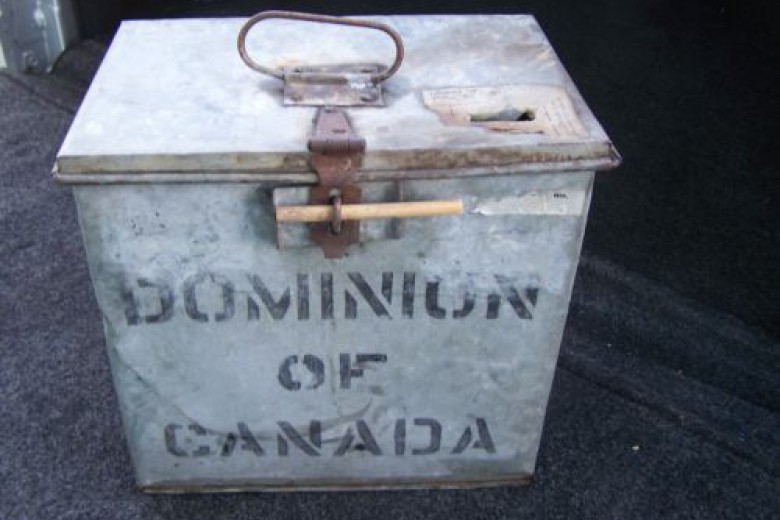
In 2002, a group of residents and advocates met at the intersection of Main and Hastings in Vancouver holding a 100-foot-long hypodermic needle made out of a giant cardboard tube, stopping traffic. They were protesting the forced closing of a needle exchange on the corner of Main and Hastings in the Downtown Eastside. Earlier, in 2001, front-line workers had distributed clean needles in a trailer outfitted with washrooms, and ensured those using in bathroom stalls didn’t overdose. Affectionately known as “the Thunder Box,” the trailer became one of North America’s first unsanctioned supervised injection sites.
These stories are among countless actions detailed in Travis Lupick’s Fighting for Space, which tells of the struggle that led to the implementation of Canada’s first official safe-injection site in Vancouver in 2003. The history of the harm reduction movement is one of direct action and protest – an “act first, ask second” attitude that was the only reasonable response to an outbreak of preventable disease and a crisis of premature deaths. Lupick focuses on the Portland Hotel Society (PHS), the groundbreaking housing non-profit that offered low-barrier housing to the city’s most vulnerable, and the Vancouver Area Network of Drug Users (VANDU), the advocacy group that pushed for accessible health care and decriminalization of drug use. The two worked in tandem, with VANDU often willingly taking the heat for direct actions to protect the more diplomatic and funding-restricted Portland Hotel Society.
The history of the harm reduction movement is one of direct action and protest – an “act first, ask second” attitude.
The 1990s saw a dramatic spike in overdose deaths and high rates of HIV diagnoses in Vancouver – not unlike the current fentanyl crisis playing out across Canada. But this time the human cost is much higher, with 2017 being the deadliest year on record for overdose deaths in B.C. The strategies used by advocates on the West Coast, honed over decades of persistent work, can provide guidance for similar struggles being newly waged in neighbouring Prairie provinces like Saskatchewan, where fentanyl has killed over 40 people since 2015.
While revealing the staggering numbers of diagnoses and deaths is key to understanding the scope of the problem, it is the stories of the people who’ve lived through the harm reduction movement that makes this history real. By telling the accounts of people struggling for dignity against politicians and a public determined to dehumanize them, Lupick reinforces two basic claims of the harm reduction movement: people who use drugs are human, and all people deserve safety and health.
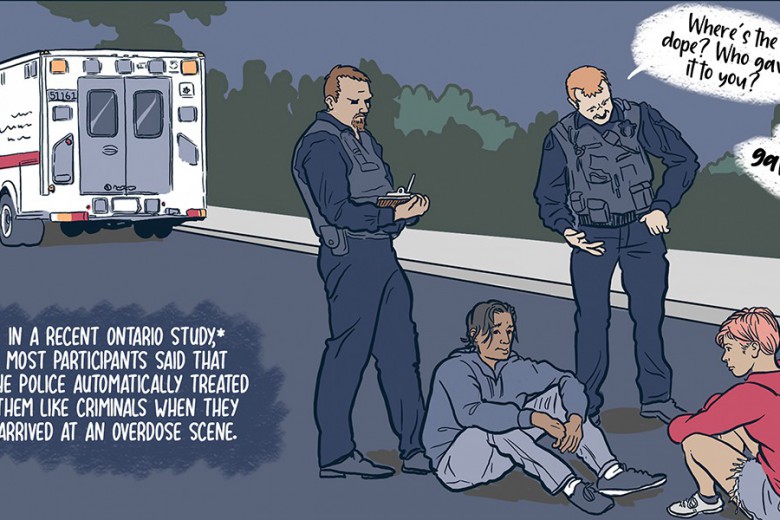
In one of their first organized meetings, members of the newly formed VANDU agreed that they wanted somewhere safe and healthy to spend time, a space that was free of police harassment. The Portland Hotel Society’s first residence was known as the “Hotel of Last Resort.” Simplifying their message to one of “health and safety” – one that politicians and the public couldn’t reasonably reject – has grounded all of their actions and successes in the harm reduction movement. Lupick concludes the book with an epilogue about a family — Mary, Molly, and Mikel — in a quietly triumphant story of three generations living in the Portland Hotel Society, all experiencing stability in their health and housing.
Lupick reinforces two basic claims of the harm reduction movement: people who use drugs are human, and all people deserve safety and health.
Lupick does not deify Vancouver’s advocates or their process – rather, he shows them to be people offering the simple necessities of safety and support, while working toward inclusive public health policy. He demonstrates a proven way to effectively build low-barrier health care and housing systems: through persistent action coupled with advocacy, and building partnerships with sympathetic policy-makers. Without this infrastructure, the number of overdose deaths in B.C. last year would have been much higher.
The current situation on the Prairies is nearly as dire as the one Vancouver faced in the 1990s. Saskatchewan’s HIV-AIDS rates are the highest in the country, and with 79 per cent of the people newly diagnosed as HIV-positive self-identifying as Indigenous, programming must prioritize consultation with Indigenous communities. Meanwhile, harm reduction programs have been heavily stigmatized by a predominantly conservative public and openly scrutinized by political leaders. In 2009, former premier Brad Wall said his government would limit the number of clean needles handed out, despite a Saskatchewan Ministry of Health report proving the success of needle exchange programs. In 2017, The Sask. Party threatened community based organizations with a 10 per cent funding cut that would hit operations deemed not to be “core services,” like needle exchanges. Though the party eventually opted against the funding cut, when harm reduction programs are routinely among the first to be threatened, the work being done by those of the front lines is delegitimized and destabilized.
When harm reduction programs are routinely among the first to be threatened, the work being done by those of the front lines is delegitimized and destabilized.
For years, doctors, front-line workers, and advocates in Saskatchewan have been pushing for the province to declare a state of emergency regarding rising HIV rates. But if we continue to wait for a provincial government to take necessary action – especially as two newly elected party leaders wade in slowly, in a province where the health of First Nations people is systematically neglected — it may never happen. Prairie activists and front-line workers struggling through those bureaucracies must instead act upon their values and conscience to build systems of equitable health care and human services, regardless of whether they have been granted permission by the state.